Why Your Weight Matters During Pregnancy
08 August 2024
Gaining weight is a natural part of pregnancy, but it's also a subject that deserves careful attention. Maintaining a healthy weight is crucial for the well-being of both mother and baby, as being either overweight or underweight can lead to complications.
In this article, we’ll cover everything you need to know about healthy weight gain during pregnancy, including recommended guidelines and potential complications associated with being at an unhealthy weight during this critical time.

How Much Weight Should You Gain During Pregnancy?
As your baby grows within you and your body undergoes changes to support new life, weight gain is expected and normal.
The amount of weight gain is different for every mother and pregnancy. Here are the general guidelines for healthy weight gain during pregnancy based on body mass index (BMI):
- Underweight (< 18.5 kg/m²): 12 - 18 kg
- Normal (18.5 - 24.9 kg/m²): 11 - 16 kg
- Overweight (25 - 29.9 kg/m²): 7 - 11 kg
- Obese (>30 - 29.9 kg/m²): 5 - 9 kg
For pregnant mothers expecting twins, a weight gain of 16 - 20 kg is considered healthy.
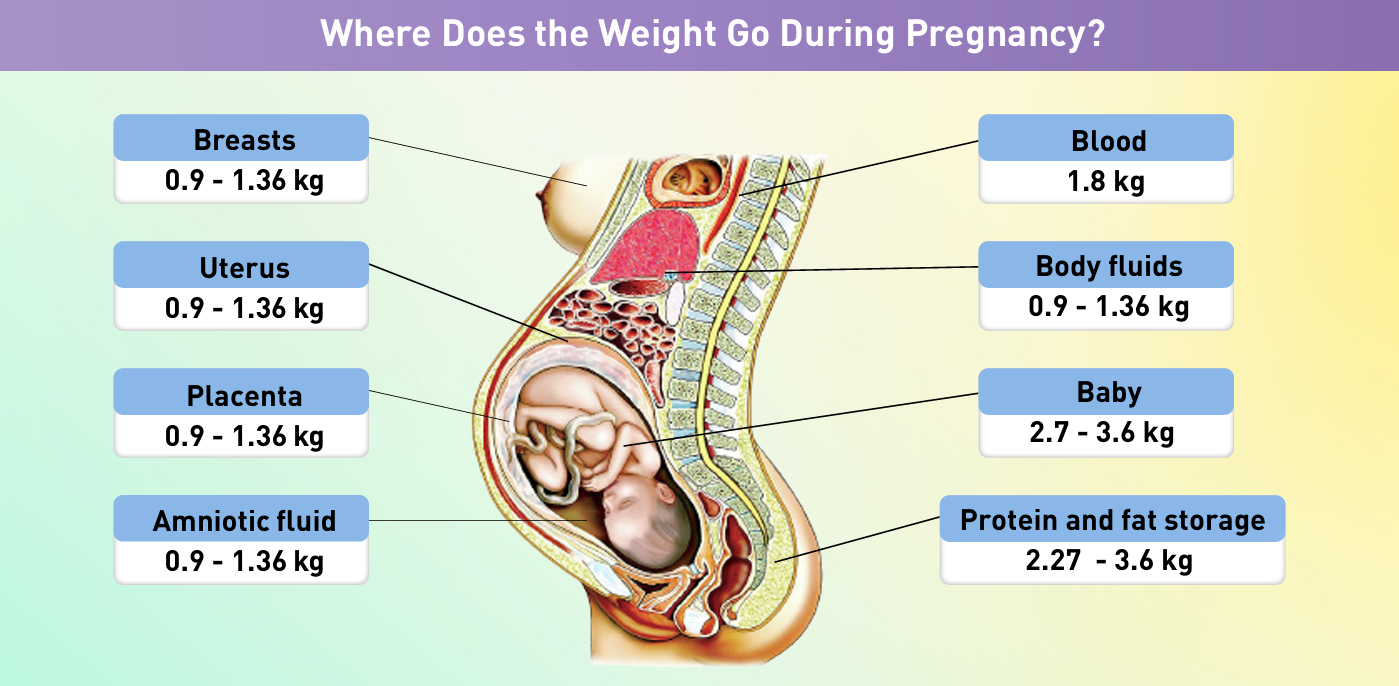
Where Does the Extra Pregnancy Weight Come From?
While your growing baby accounts for some of the weight gain during pregnancy, other changes to your body as it accommodates your baby’s growth also contribute significantly.
Here is an breakdown of what contributes to the pregnancy weight gain:
- Breast: 0.9 - 1.36 kg
- Uterus: 0.9 - 1.36 kg
- Placenta: 0.9 - 1.36 kg
- Amniotic fluid: 0.9 - 1.36 kg
- Blood: 1.8 kg
- Body fluids: 0.9 - 1.36kg
- Baby: 2.7 - 3.6 kg
- Protein and fat storage: 2.27 - 3.6 kg
What Are the Risks of Being Overweight During Pregnancy?
Being overweight during pregnancy can increase the chances of complications for both the mother and the unborn baby. The higher your BMI while pregnant, the greater the risk of encountering complications such as:
- Gestational hypertension and pre-eclampsia
- Gestational diabetes
- Delivery complications
For the baby, risks include:
- Macrosomia, which refers to newborn weighing more than 4.0 kg at birth
- Congenital anomalies (e.g., spina bifida, cleft lip)
- Preterm birth
- Stillbirth
What Are the Risks of Being Underweight During Pregnancy?
Being underweight during pregnancy also poses risks. It can lead to potential complications for the mother, including:
- Anaemia
- Osteoporosis
- Delivery complications
- Premature rupture of membranes (PROM)
A baby born to an underweight mother faces an increased risk of these complications:
- Preterm birth
- Neonatal Intensive Care Unit (NICU) admission
- Low birth weight or intrauterine growth restriction (IUGR)
Exploring Complications Associated with Weight During Pregnancy
Gestational Diabetes
Gestational Diabetes is a condition characterised by high blood sugar levels that develop during pregnancy and typically resolve after giving birth.
It can occur at any stage of pregnancy. However, it is more common in the second half of your pregnancy. It occurs when your body cannot produce enough insulin — a hormone that helps control blood sugar levels — to meet the increased demands of pregnancy.
Who Is at Risk?
While any woman can develop gestational diabetes during pregnancy, the risk is higher if you:
- Have a BMI above 30
- Previously had a baby who weighed 4.0 kg or more at birth
- Have a history of gestational diabetes during pregnancy
- Have a family history of diabetes
- Have family origins in South Asian, Chinese, African-Caribbean or Middle Eastern backgrounds
Complications of Gestational Diabetes
Potential complications include:
- Macrosomia which refers to newborn weighing more than 4.0 kg at birth
- Neonatal hypoglycaemia, or low blood sugar in the newborn
- Neonatal jaundice,
- Foetal respiratory distress syndrome (FRDS), a condition when a newborn’s lungs are not fully developed and cannot provide enough oxygen
- Preterm delivery
- Increased risk of developing type 2 diabetes later in life
Hypertensive Disorders Of Pregnancy
Hypertensive disorders during pregnancy include a range of conditions that can be classified into several categories:
- Chronic Hypertension: Usually diagnosed before 20 weeks’ gestation or is first diagnosed during pregnancy and persists beyond 12 weeks postpartum.
- Gestational Hypertension: Diagnosed after 20 weeks' gestation, with blood pressure of more than 140/90 mmHg but no presence of protein in urine or signs of severe pre-eclampsia.
- Pre-eclampsia: Develops after 20 weeks' gestation, with blood pressure more than 160/90 mmHg, presence of protein in urine or evidence of organ injury.
- Chronic HTN + Pre-eclampsia: Marked by a sudden increase in blood pressure that was under control, with new onset of protein or sudden increase of protein levels in urine with no previous history of its presence.
- Pre-eclampsia+
- Preeclampsia with Severe Features: Presence of systolic blood pressure more than 160mmHg, diastolic blood pressure of more than 110mmHg or any organ injury
- Eclampsia: The development of tonic-clonic seizures with severe pre-eclampsia.
- HELLP Syndrome: Characterised by haemolysis, elevated liver enzymes and low platelets associated with preeclampsia or eclampsia.
Who Is at Risk?
Women who are at an increased risk of hypertensive disorders of pregnancy include those who:
- Have a BMI above 30
- Consume alcohol
- Have a history of heart failure or stroke
- Have a family history of hypertension
- Have left ventricular hypertrophy
- Smoke
Complications of Hypertensive Disorders of Pregnancy
Possible complications include:
- Placental abruption
- Harm to mother’s kidneys and other organs
- Preterm delivery, intrauterine growth restriction or low birth weight
- Postpartum eclampsia (within the first 48 hours post-delivery)

Anaemia During Pregnancy
Anaemia during pregnancy is diagnosed when haemoglobin levels fall below 11g/dl. Anaemia can be categorised into:
- Mild: 10.0 – 10.9 g/dl
- Moderate: 7.0 – 9.9 g/dl
- Severe: Less than 7.0 g/dl
Maternal anaemia has significant adverse effects on both mothers and babies. The risk of death among pregnant women with severe anaemia has been reported to be twice that of mothers without severe anaemia.
Who Is at Risk?
Women at higher risk of anemia during pregnancy include those who:
- Have an existing anaemia condition
- Struggle to maintain iron supplement intake
- Booked late for antenatal care
- Have had multiple pregnancies
- Are of Indian ethnicity
Complications of Maternal Anaemia
The adverse effects of maternal anaemia include:
- Perinatal death
- Neonatal iron deficiency
- Preterm delivery or low birth weight
- Heart failure
- Postpartum depression

Managing your weight during pregnancy is vital for the health of both you and your baby. By understanding the recommended weight gain guidelines and the risks associated with being either overweight or underweight, you can take proactive steps to support a healthy pregnancy.
Stay connected with your Consultant Obstetrician and Gynaecologist to ensure you're on the right track, and make choices that promote a positive outcome for you and your baby.
If you are looking for a Consultant Obsterician and Gynaecologist to journey with you and monitor you and your baby’s health as well as well-being through your pregnancy journey, get started here.
References:
- Dr. Zainab bt. Kusiar. 2012. Nutrition during pregnancy. MYHEALTH MINISTRY OF HEALTH MALAYSIA; Institute of Medicine and National Research Council (2009)
http://www.myhealth.gov.my/en/nutrition-during-pregnancy/ - Subramaniam et al. 2017. Gestational diabetes mellitus: The prevalence, associated factors and foeto-maternal outcome of women attending antenatal care. Malaysian Family Physician. 12(2).
- Brown MA et al. 2018. Hypertensive Disorders of Pregnancy: ISSHP Classification, Diagnosis and Management
Recommendations for International Practice. 72: 24 – 43. - Abd Rahman R et al. 2022. The Prevalence and Risk Factors of Iron Deficiency Anemia Among Pregnant Women in Malaysia: A Systematic Review. Front Nutr. 9: 847693






