Safe Use of Antibiotics
Antibiotics Are NOT Always the Answer
Most cough and cold illnesses are caused by viruses. Antibiotics can only treat bacterial illnesses–not viral illnesses.
Common illnesses where antibiotics are NOT REQUIRED include:
Colds
Influenza
(the flu)
Runny noses
Most coughs
Most sore throats
Most sinus infections
Some ear infections
How long will the symptoms last?

Sore throat / tonsillitis: 1 week

Cold / flu: 10 days – 2 weeks

Runny / blocked nose: 1 – 3 weeks

Sinusitis: 2 – 3 weeks

Dry / tickly cough: 3 weeks
If symptoms last longer than normal, do not improve, get worse or if new symptoms develop, seek medical advice.
Get SMART on Antibiotics


Lozenges

Sprays

Gargles

Tablets

Solubles

Syrups

Drops
How do I know if I have a viral or bacterial infection?
Consult healthcare provider and follow his or her advice on what to do about the illness. Remember, common colds are caused by viruses and do not require antibiotics.
Does this mean I should never take antibiotics?
Your healthcare provider will prescribe antibiotics if you have a bacterial infection.
If mucus from nose changes from clear to yellow or green – does this mean that I need antibiotics?
No. It is normal for mucus to get thick and change colour during a viral cold.
What can I do to help myself feel better?
Pain relievers, fever reducers, saline nasal spray or drop, warm compress, liquids and rest may be the best things to help you feel better.
References:
Snort. Sniffle. Sneeze. No Antibiotics Please. Centres for Disease Control and Prevention (CDC).
Get to the source of Cold & Flu symptoms. Global Respiratory Infection Partnership (GRIP).
Upper Respiratory Tract Infections Getting the right relief. Global Respiratory Infection Partnership (GRIP).
Antibiotic Awareness - What You Should Know
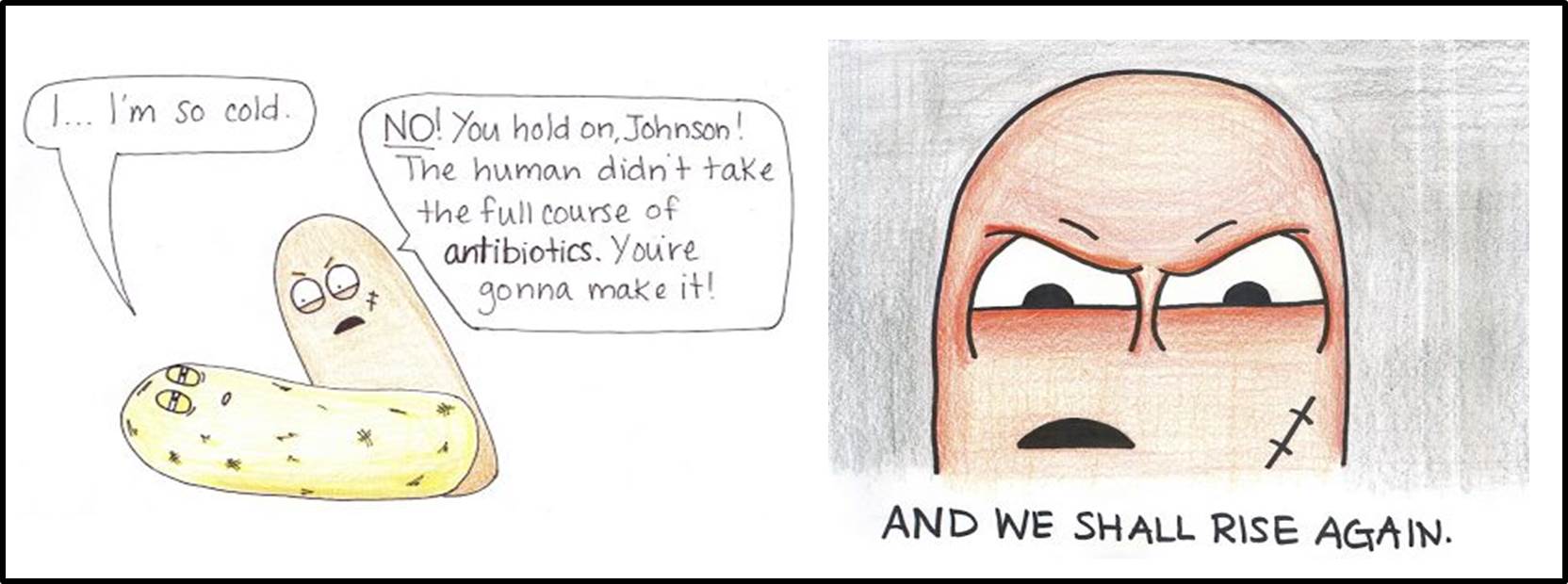
Why should I finish my antibiotic?
Not finishing a course of antibiotics as directed can lead to *antibiotic resistance.
* Antibiotic resistance is resistance of the bacteria to the antibiotic that was originally effective for treatment of infections caused by it. Illnesses that were once easily treatable with antibiotics become dangerous infections, prolonging suffering and may even be fatal.
YOU can help tackle resistance by:
- Hand washing and avoiding close contact with sick people to prevent transmission of bacterial infections;
- Use antibiotics only when they are prescribed by a certified healthcare professional;
- Completing the full treatment course, even if you feel better;
- Never share antibiotics with others or use leftover prescriptions
I developed diarrhoea after taking antibiotics. Should I stop it?
In some patients, antibiotics may cause mild diarrhoea, which is a well known effect. You do not need to discontinue your antibiotic but well hydrate yourself to replace the lost fluids and avoid milk containing products.
Probiotics are recommended to help with diarrhoea. However if you develop severe abdominal pain, cramps or fever with high volume diarrhoea after taking antibiotics, you should seek your doctor’s attention immediately.
I developed an allergic reaction towards penicillin. Is it safe for me to take other antibiotics?
If you developed itchiness, difficulty breathing and/or wheezing after taking penicillin, then you are allergic to it and you should not take any product containing penicillin or an antibiotic of a similar class.
It is important that you notify any doctor or pharmacist that looks after you on your allergy status. There are other antibiotics available which are safe to use for people with penicillin allergy.
References:
https://www.drugs.com/health-guide/antibiotic-associated-diarrhea.html
http://www.who.int/drugresistance/en/
http://www.cdc.gov/getsmart/community/about/antibiotic-resistance-faqs.html






