If you have had a stroke, a dedicated team of health professionals is here to care for you from the very beginning till you recover to your fullest potential.
The goal of stroke rehabilitation is to restore as much independence as possible by improving physical, mental and emotional functions. This must be done in a way that preserves your dignity and motivates you to re-learn skills that the stroke may have affected.
What Is Stroke?
A stroke is caused when the flow of blood to the brain is stopped by:
- a blocked blood vessel (ischemic stroke); or
- a burst blood vessel causing a bleed into the brain (hemorrhagic stroke).
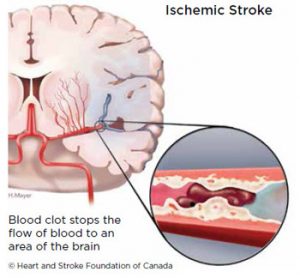
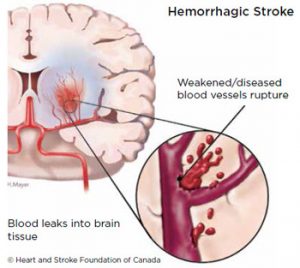
As a result, brain cells do not receive the oxygen and nutrients they need to work normally. Some brain cells become damaged and others die. It is not always possible to know what caused a stroke. Every stroke is different.
On the other hand, TIA (Transient Ischemic Attack) or mini-stroke produces sudden and brief stroke-like symptoms (usually only for a few minutes) but it will usually recover within 24 hours and will not cause any obvious disability or permanent brain damage. However, TIA, can act as a ‘warning’ that one could potentially have a more damaging stroke in the future and should be taken seriously.
After history taking and examination, a hospital admission would usually follow. A number of tests may be done:
- Brain scan to confirm type of stroke and location:-
- CT scan (Computed Tomography) – this can show the kind of stroke you have had and how much damage it may have caused.
- MRI scan (Magnetic Resonance Imaging) – this can give a more detailed picture of your brain. It is sometimes used instead of a CT scan for certain types of strokes, or to make sure what was found in the CT scan is correct.
- Blood tests to look for underlying diseases such as diabetes and high cholesterol.
- Chest X-ray and Electrocardiogram (ECG) to evaluate lung and heart condition.
- Ultrasound studies to assess blood vessels.
- Angiogram to test severity of vessel blockage.
The signs and symptoms of a stroke depend on the area of the brain that is affected and how much damage there is. Different parts of our brain control different body functions. Common signs and symptoms include:
- sudden numbness or weakness of the face, arm, or leg especially on one side of the body
- loss of movement and / or sensation down one side of the body
- sudden trouble walking, clumsiness, dizziness, loss of balance or coordination
- communication and language problems
- cognitive difficulties e.g. concentration, memory
- sudden vision loss
- swallowing difficulties
- loss of bladder / bowel control
- sudden severe headache
- psychological changes e.g. anxiety, depression
- tiredness
Prevention
There are two types of risk factors, namely modifiable and unmodifiable risk factors. Modifiable risk factors are contributors that you can control or manage to reduce your risk for a stroke.
Modifiable Risk Factors
- Uncontrolled hypertension (high blood pressure)
- High cholesterol
- Diabetes
- Poor diet and sedentary lifestyle
- Regular heavy drinking
- Smoking
- Oral contraceptive pills
- Atrial fibrillation (irregular heartbeat)
Unmodifiable Risk Factors
- The risk for a stroke increases with age
- Males have an increased risk of getting a stroke
- Family history of stroke
Speak to your doctor/healthcare professional to learn more about your risk for a stroke and how to manage the risk factors.
Some signs to look out for when identifying an occurrence of a stroke include:
BALANCEDoes the person have a sudden loss of balance? |
|
EYESDoes the person have vision loss or blurred vision in one or both eyes? |
|
FACEDoes the person’s face look uneven? |
|
ARMIs one arm hanging down or weak? |
|
SPEECHDoes the person have trouble speaking clearly or seem confused? |
|
TIMEIf you suspect it is a stroke, call 999 or get to a hospital as fast as you can! |
Have a balanced diet
Changing your diet habits can make a huge positive impact to your overall health. Some tips for healthy eating are limiting the intake of salt, sweets and sweetened beverages, eating lots of fruits, vegetables and whole grains and limiting saturated fats and trans fats. Many times, these rules are widely known but not widely practised. So start eating healthy today!
Exercise regularly
Keeping active has been known to reduce the risk of a stroke. The American Heart Association recommends
- walking a minimum of 10,000 steps per day,
- 150 minutes moderate-intensity or 75 minutes high-intensity exercise per week, in order to maintain a healthy heart. A healthy heart reduces the risk of getting a stroke.

Manage chronic diseases
Diabetes, hypertension and high cholesterol are known to increase your risk for a stroke. Consult your doctor to understand more about these conditions and the medicines that can help you control them.
Quit smoking
Quitting smoking may require some discipline and determination on the smoker’s side. However, there are some aids that can help you in your effort to quit smoking such as the nicotine patch and gum. Talk to your doctor/pharmacist for options to help you quit smoking. SunMed Pharmacy offers private and personalized quit smoking consultations. For more information, visit: https://sunwaymedical.com/en/quit-smoking/

Manage your stress level
Emotional stress can lead to hypertension through the release of stress hormones in your body. Some common ways to alleviate stress are engaging in your favourite activities, exercising or sharing your problems with family or trusted friends. Seek professional help if you feel that you are unable to manage the stress on your own.
Recovering From Stroke
Brain cells do not regenerate post stroke. However, the brain is somewhat flexible and is able to reorganize itself to an extent, in order to regain lost function. This however needs the Stroke survivor to engage in rehabilitative activities that help these alternative pathways to develop.
Timescales for recovery and rehabilitation after stroke
Commonly speaking, the first six months post stroke are deemed the “optimal recovery period” where rapid recovery can take place and when rehabilitation is of utmost importance. Six months after the injury the picture will be clearer as to how much recovery is possible. However, studies have shown that it is still possible to recover after 1 year post stroke, with organized, intensive Rehabilitation.

The Lokomat Pro V5® is an advanced Neuro Rehabilitation training device that provides highly repetitive and the most physiological gait training – especially to severely impaired patients. More info here.
Where does Rehabilitation take place?
| Inpatient rehabilitation | This involves intensive specialist rehabilitation for patients who are still hospitalised and who are not ready to return home after discharge from acute care. |
| Outpatient rehabilitation | Some patients may be well enough to return home and receive further treatment as an outpatient, either at a local hospital or at a separate rehabilitation centre. |
| Community rehabilitation | Following an inpatient rehabilitation stay, some patients may be transferred to a residential transitional living unit or may go straight back to their homes, with a community rehabilitation team or outreach team helping them to make further progress in developing independent living skills. |
Physical weakness
Weakness on one side of the body (depending on the site of the stroke) is a common complication post-stroke. Active rehabilitation, e.g. mobilisation and exercises, is important to help you regain physical functions. Occupational Therapists (OTs) may fabricate rehabilitative aids such as ankle-foot orthosis and wrist-hand orthosis to prevent abnormal positioning and contractures of joints on the paralysed side.

Bed or Pressure Sores
Sores usually appear on the elbows, buttocks or heels due to prolonged lying or sitting. The stroke survivor should not sit or lie in the same position for long periods of time.
Shoulder Care
Frozen shoulder is a common condition after stroke. Never pull a stroke survivor by the arm to avoid shoulder dislocation.
Communication Problems
Losing the ability to speak or understand can be frustrating. You may find it encouraging knowing that many patients improve over time, through therapy. A stroke survivor needs to be given time. If you are looking after a person with stroke, you may need to speak slower than usual, and speak in shorter sentences.
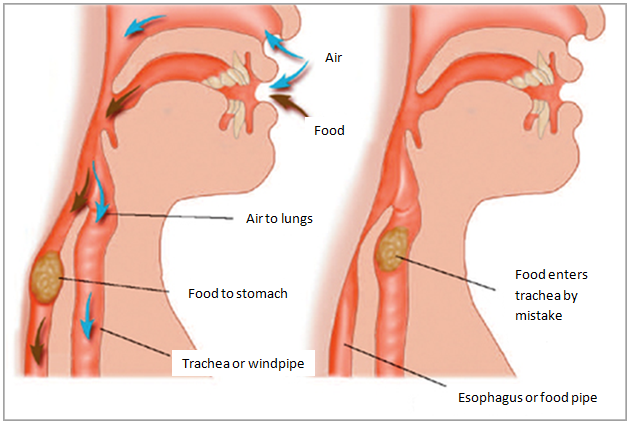
Swallowing Problems
After stroke, a person may experience difficulty to eat and drink safely or with ease. Swallowing difficulties may lead to aspiration, in which food /drinks travels into the lungs, resulting in a chest infection (or termed aspiration pneumonia).
A speech-language and swallowing therapist may recommend diet modification and swallowing strategies to ensure safe swallowing.
Continence Problems
Problems with bowel or bladder control are very common after stroke. Up to one half of the stroke patients may have incontinence. Though this can be very distressing, many of these problems will resolve over time.
Emotional Changes
Studies suggest that around 30% of stroke survivors experience mood changes (e.g., depression) after stroke, which could affect their recovery process and quality of life. In addition, caregivers may suffer from caregiver stress. Consult your doctor or clinical psychologist for assessment and management strategies.
Behavioural and Personality Changes
Apart from the psychological effects, some stroke survivors may go through behavioural changes due to the damage to the brain. They may become irritable and aggressive or withdrawn and passive. The stroke survivor may not recognise that their personality has changed.
Memory Loss
Family members may notice that the patient may be asking the same questions repeatedly or is not able to remember details of recent events. Many patients do recover from memory loss. Cognitive stimulation therapy is important for better cognitive abilities such as attention and memory skills.
About your medications:
- Always take your medications as prescribed.
- Take your medications at the same time every day.
- Do not stop taking your medications without discussing with your doctor or pharmacist first.
- Keep an up-to-date list of your medications with you at all times.
- Do not take any over-the-counter medications, supplements, vitamins or herbs without asking your doctor or pharmacist first.
- If you have any questions about your medications, talk to your doctor or pharmacist.
- If a medication is causing unpleasant side effects, report them to your doctor or pharmacist. Sometimes your doctor can help you to eliminate side effects by simply changing the dose, suggesting that you take the medication at a different time or change to a different medication.
Common Medicine Used in Stroke Care
| Antiplatelets |
These drugs are used to prevent platelets from sticking together, and thus prevent blood clots from forming. Blood clots can block blood flow to your brain, causing a stroke. Examples of antiplatelets are:-
|
| Anticoagulants | These drugs prevent new blood clots from forming and existing blood clots from getting bigger. They work by increasing the time it takes for your blood to clot. If you have a type of irregular heartbeat called atrial fibrillation and you have had a stroke, taking an anticoagulant can lower your risk of having another stroke. |
| Antihypertensives | These drugs are used to lower your blood pressure. It is important to have your blood pressure checked regularly as high blood pressure increases your risk of having another stroke. |
| Lipid regulators & Statins | These drugs are used to lower your LDL cholesterol (often referred to as ‘bad’ cholesterol) levels, and thus your risk of having another stroke. They work by reducing the production of cholesterol in your liver. |
| Diabetic patients | If you have diabetes, it is important for you to take your diabetic medication as instructed by the doctors, and keep your blood sugar as near normal as possible. Good control of blood sugar reduces the risk of having another stroke. |
Follow-up with the doctors
Follow-up is an important part of rehabilitation. Visit your doctors routinely to allow detection and management of high blood pressure, diabetes mellitus, high cholesterol and heart diseases.
Nutrition
After a stroke, you need to get sufficient nutrients to enhance your recovery. Furthermore, healthy eating to manage your blood pressure, cholesterol, blood sugar and body weight is also important to reduce your risk of having another stroke.
Healthy eating after stroke
- Eat at least 5 servings of fruits and vegetables daily.
- Incorporate whole grains and high fibre food varieties into daily meals such as oats and brown rice.
- Choose lean protein such as fish, lean meats, egg, soy bean curd and beans. Eat fish at least twice a week.
- Choose healthy cooking method such as steaming, grilling, and boiling.
- Limit saturated fat intake such as animal fat/skin, butter and coconut milk.
- Cut down trans fat such as fried food and food products that contain partially hydrogenated oil (cookies, crackers and baked goods).
- Cut back on drinks and foods with added sugar.
- Limit intake of salt and processed foods.
- Limit your alcohol intake to no more than one drink per day.
If you are unable to swallow food or fluids safely or adequately, you may need tube feeding. Tube feeding is the delivery of nutrients through a tube to the body e.g. a nasogastric tube. The dietitian will advise you on the amount of balanced nutrition supplement that you need.
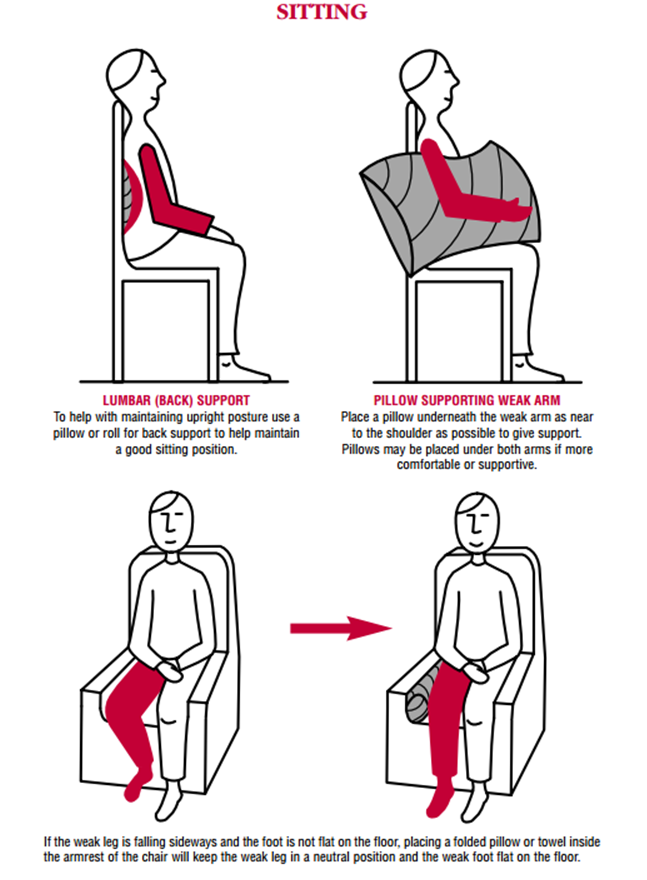
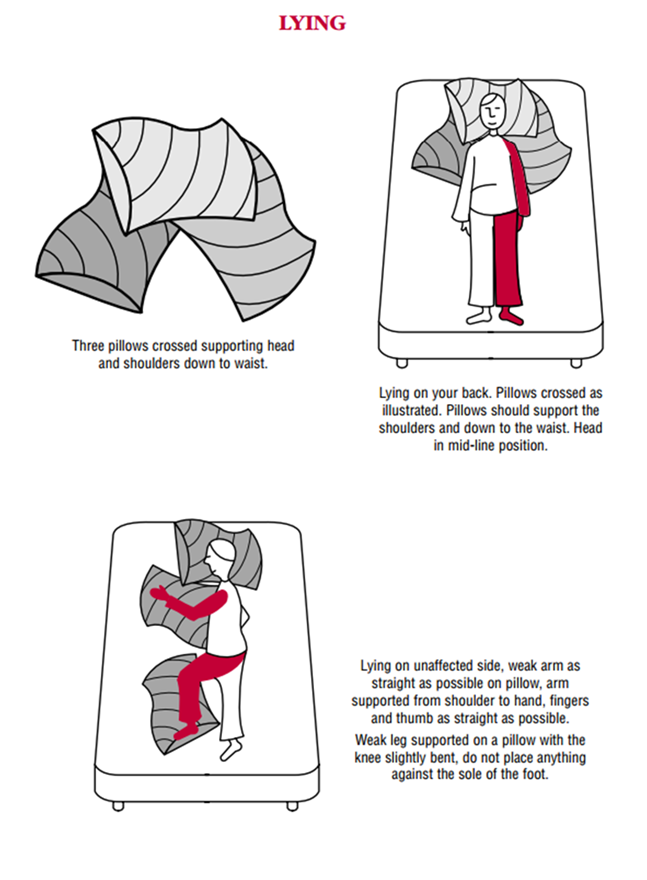
Positioning, mobilisation and exercises
The physiotherapists will advise you on how you should be positioned, when lying or sitting. If you have one-sided paralysis, correct positioning is important to prevent spasm or injury.
You may also be trained to sit out of bed in a chair for increasing periods of time. Eventually, the rehabilitation will move on to re-education of walking.
Exercise plays an important role in the recovery from stroke. You should practise the exercises that are taught by your therapists regularly to improve your physical functions.
Activities of Daily Living
After stroke, you are encouraged to continue with your previous activities, for example, dressing and feeding yourself as much as you are able to. After identifying the difficulties you have with everyday tasks, your occupational therapist can help by either teaching a different way to complete the activity, recommending changes that will make the activity easier or by providing devices that make activities easier.
Studies show that 80-90% of patients will survive after a stroke. Brain cells that have died will not heal. However, other parts of the brain can take over the functions of the areas that are damaged. When this happens, we see recovery of body functions in stroke survivors.
Recovery takes time. As such, do not lose hope if the effect of stroke appears severe in the beginning. Participate in all the rehabilitation exercises recommended by your stroke rehabilitation team.
The Stroke Care Team
Being in the company of stroke survivors and their families are reassuring. Below are some resources for you and your family:
SunMed Stroke Caregivers Club
Stroke Caregivers Club is a support group that provide the stroke survivors and their family members a platform to access to information and support from not only clinicians but also other stroke survivors and their family members.
Please enquire our Stroke Care Team for our next meeting date and details. Admission to meetings is free.
Here for you 24/7
| Stroke Hotline | +6019-378 0119 |
| For Ambulance | +6019-666 6940 |
| For General Enquiries | +603-7491 9191 |